The solution assists with unifying and visualizing disparate data, providing population health management, improving health equity and omni-channel patient engagement.
The solution assists with unifying and visualizing disparate data, providing population health management, improving health equity and omni-channel patient engagement.
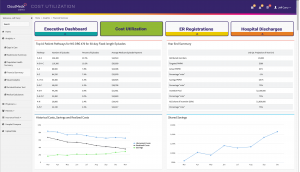
CloudMedx’s ACO REACH Explorer is a bundled solution suite that provides support for the full spectrum of ACO REACH requirements. This includes unifying and visualizing disparate data (via the ONE Platform), providing population health management (via Clinical Explorer), improving health equity (via SDOH Explorer) and omni-channel patient engagement (via Patient Explorer). The bundled solution is specifically tailored for the ACO REACH participants, providing a seamless technology suite to meet all their requirements. The insights are also available as APIs that can be integrated with existing solutions.
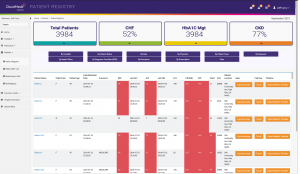
The ACO REACH is the first model launched by CMS that puts a strong emphasis on health equity. All ACOs in the model will have to develop a plan for how they will identify health disparities in their respective communities and then take specific actions to address those disparities.
The CloudMedx ACO REACH Explorer has all the functionality of SDOH Explorer (https://sdohexplorer.cmxcloud.com/) and Chronic Conditions Explorer embedded into it. This includes:
All of the features are essential as ACOs’ financial spending targets will be higher and easier to hit if they serve the most socially and economically at-risk patients. Conversely, ACOs that serve the least at-risk patients will have their benchmarks slightly lowered.
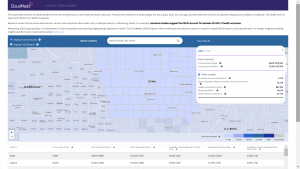
CloudMedx’s ONE Platform aggregates and normalizes incoming data sets (clinical data, social determinants of health data, healthcare claims and payment data) and unifies that data in a single data visualizing layer. All incoming data is ingested in an automated manner – driving efficiencies and reducing burden on staff.
The ONE Platform is the core for each application – with a great infrastructure and clean data at the heart of the system – ensure smooth operations and complete insights.
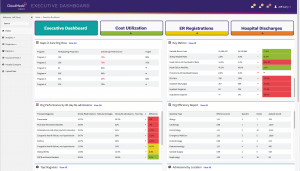
The ACO REACH Explorer includes CloudMedx’s population health management tool that
Risk adjustment module is also bundled in the CloudMedx ACO REACH Explorer. It assists with the following capabilities
For more details on CloudMedx’s RA Analyzer, please click here
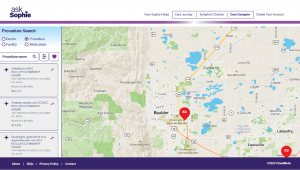
ACOs can prevent network leakage and quickly and easily pair patients with in-network specialists. It provides intuitive mapping and customizable specialist criteria to ensure a seamless referral network management.
It also assists care teams in targeted outreach to improve member experience and reduce costs. Some of key features include: